ESP Disc Replacement
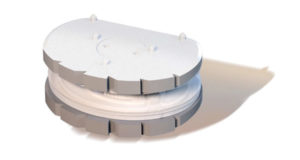
The ESP Disc Replacement is a mono-bloc total disc replacement implant that restores natural disc functions.
The ESP disc replacement is made of 2 titanium alloy end-plates and an elasto-meric cushion. The spikes on the end-plates outer surfaces improve primary fixation. The combination of a hydroxyapatite (HA) coating on top of a T40 rough surface are considered as one of the best existing coating. The titanium alloy used for the end plates allows clear medical imaging and guarantees good bony fixation over time.
- Between the 2 titanium end-plates the elsatomeric parts are injected for controled resistance to compression, flexion and rotation. These elastomeric parts are concentric and their fixation prohibits micro motion. The materials used for the implants have been tested for biocompatibility according to the ISO standard 10993.
- Minimally invasive anterior approach which allows reduced hospital stay and improves rehabilitation
- Tested up to 40 million cycles
- ESP should give a significant reduction in pain severity, re-establish lumbar curvature and natural disc functions
- ESP allows quick return to normal daily activities
Origin of the ESP Disc Replacement
Concept of a “Silent Block” ESP®
The development of the ESP disc range originally came from Professor Roy Camille, from La Pitié Salpétrière Teaching Hospital in Paris (France). After inventing the pedicle screw which became the gold standard for Spine fusions, Pr. Roy Camille started to work on analysing the natural disc properties and designed a prosthesis to restore these.
Third generation disc replacements
Both CP-ESP and LP-ESP belong to the 3rd generation of disc replacements. Their specific mono-bloc design resulting from over a decade development allows them mimic the properties of natural discs. They provide movements in all directions without any friction and without any risks of debris production nor dislocation.
The lumbar ESP Disc Replacement
LP-ESP
The LP-ESP cervical disc replacement has been developed to mimic the natural lumbar disc and allow the spine to behave as if the replaced disc would be natural in all situations.
- Over 10 years of research and development
- 10 years of follow up (since 2004)
- 6° of freedom
- Adaptive center of rotation
- No surface bearing for an increased lifetime
- Improved stability
- shock absorbing
- Designed to fit and restore patient lordosis
Structure of the LP-ESP® Lumbar Disc Replacement
- Titanium endplates TA 6V ISO 583213 and hydroxyapatite coating
- Inner core (Silicone nucleus)
- Outer core (Polycarbonate urethane annulus)

The Cervical ESP Disc Replacement
CP-ESP
The CP-ESP cervical disc prosthesis has been developped to mimic the natural cervical disc and allow the spine to behave as if the replaced disc would be natural in all situations.
Specifics
- Heights from 5mm to 7mm
- Benefits from over 10 years of development
- 6 degrees of freedom
- Adaptive center of rotation
- No surface bearing for increased lifetime
- Improved stability
- Shock absorbing

Other natural elasto-meric non-articulating devices:
Spinal Kinetics M6 > >
Disc Replacement Surgeon
Dr. Ritter-Lang > >
